There is a direct correlation between access to health care and cancer rates, as well as correlative data linking access to quality care with better health outcomes in general. Healthcare access in the US is a financial burden and illustrates the inequitable distribution of life-saving resources across communities and demographics. Today, 1 in 10 Americans lack health insurance. Without it, families and individuals are less likely to have a primary care provider, seek preventative care or access medical treatment despite acute or chronic symptoms of disease and illness. This includes skipping recommended age-based or risk-based cancer screenings.
The Key Barriers to Healthcare Access
By 2040, the cost of inequitable access to care in the US will exceed $1 trillion. Costs associated with treating high-risk and high-cost diseases, including cancer, will put hundreds of thousands of lives at risk due to healthcare disparities caused by financial, geographic and cultural barriers. The key barriers to healthcare are:
- Insurance coverage. Millions of Americans lack any form of health insurance, but millions more are underinsured. Insufficient coverage can discourage families from seeking preventative screenings, making dental and optical appointments or accessing pediatric care due to financial constraints.
- Long waiting time. Healthcare employment challenges have left many facilities understaffed, leading to wait times that range from weeks to months. Staffing shortages are expected to last more than a decade, with American Medical Colleges predicting a shortage of 124,000 doctors by 2034.
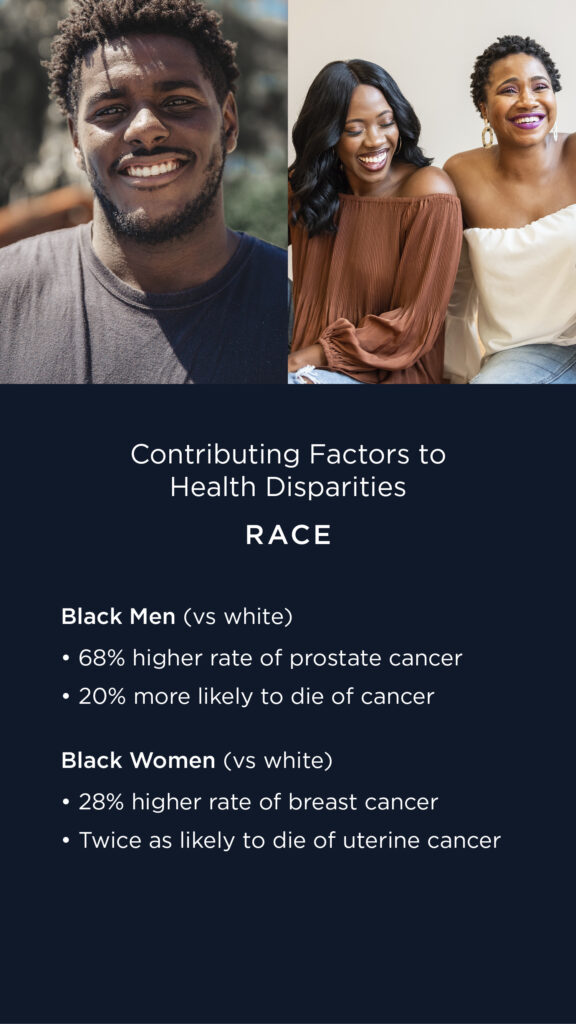
- Bias and discrimination. There is a persistent bias in the medical community that discriminates against patients based on racial, income, gender and sexual orientation. This stigma has discouraged access to healthcare services, including for those seeking mental health support.
- Time. Transportation and work duties severely restrict the time to seek care. Many programs offer transportation support to seniors or those without reliable access to transportation, but there are potentially millions in need of additional help. Telemedicine offers an important opportunity to reduce time and transportation burdens on working families.
- Language. Today, 1 in 5 American households speak a language other than English. Medical facilities lack widespread language resources that can result in frustration, misdiagnosis and discourage patients to seek care.
View the Healthcare Access Slideshow
HEALTH ACCESS CITATIONS
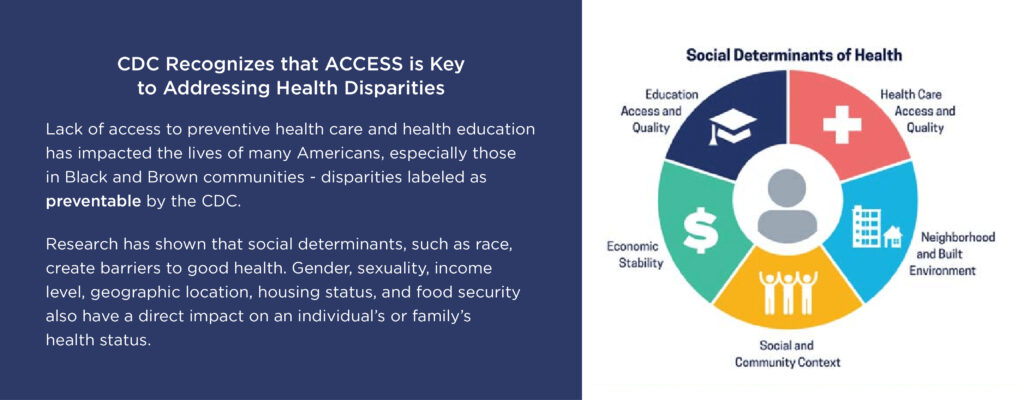
Slide #2
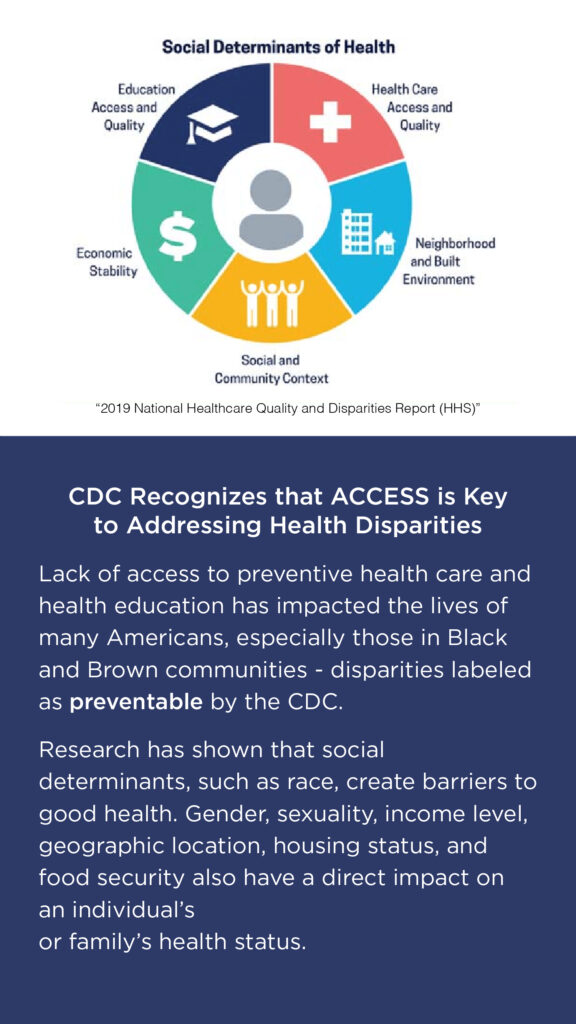
Graphic – “2019 National Healthcare Quality and Disparities Report (HHS)”
Citation: https://www.ahrq.gov/sites/default/files/wysiwyg/research/findings/nhqrdr/2019qdr.pdf “as preventable by the CDC.”
Citation: CDC. Community Health and Program Services (CHAPS): Health Disparities Among Racial/Ethnic Populations. Atlanta: U.S. Department of Health and Human Services; 2008
https://www.cdc.gov/healthyyouth/disparities/index.htm
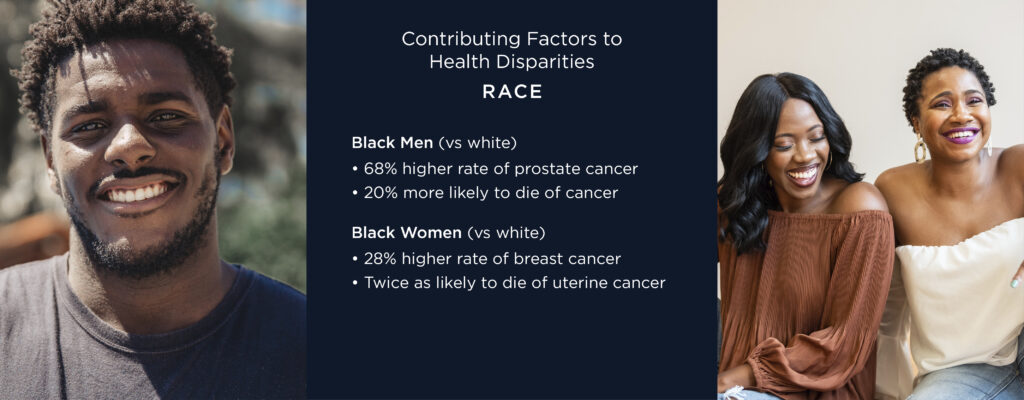
Slide #4
Slide #5
Citation: To hear more from Dr. Hanna-Attisha, please visit the Less Cancer podcast episode on Environmental Exposure Factors
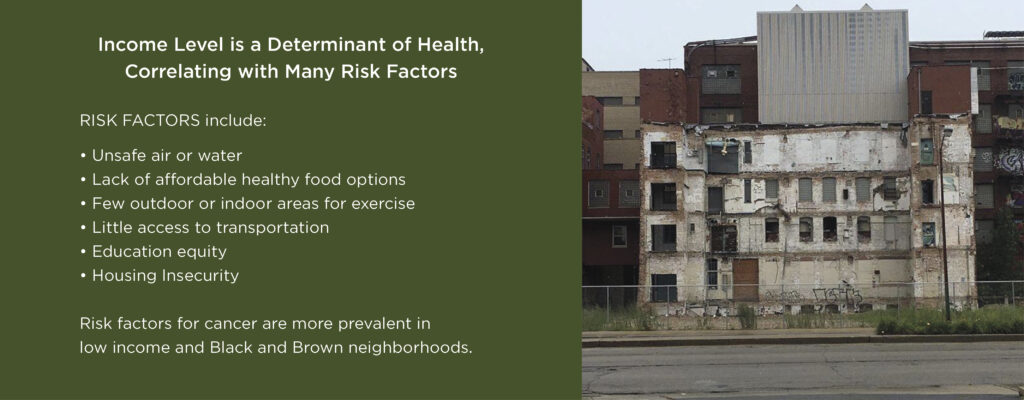
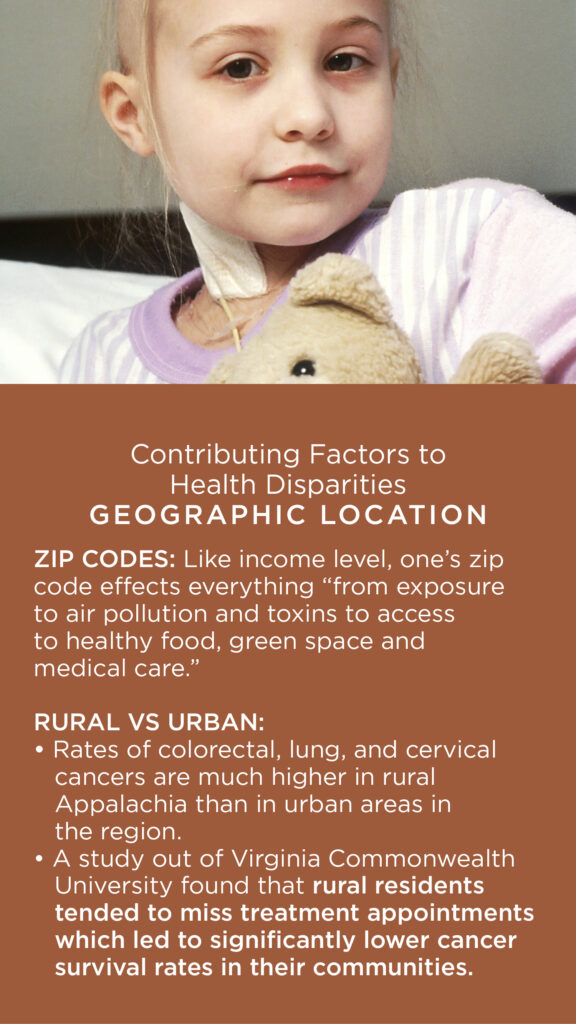
Slide #9
Citation: https://time.com/5608268/zip-code-health/
Citation: https://www.cancer.gov/about-cancer/understanding/disparities#contributing-factors
Citation: https://www.redjournal.org/article/S0360-3016(22)00638-1/fulltext
Slide #10
Citation: https://www.cdc.gov/cancer/obesity/index.htm
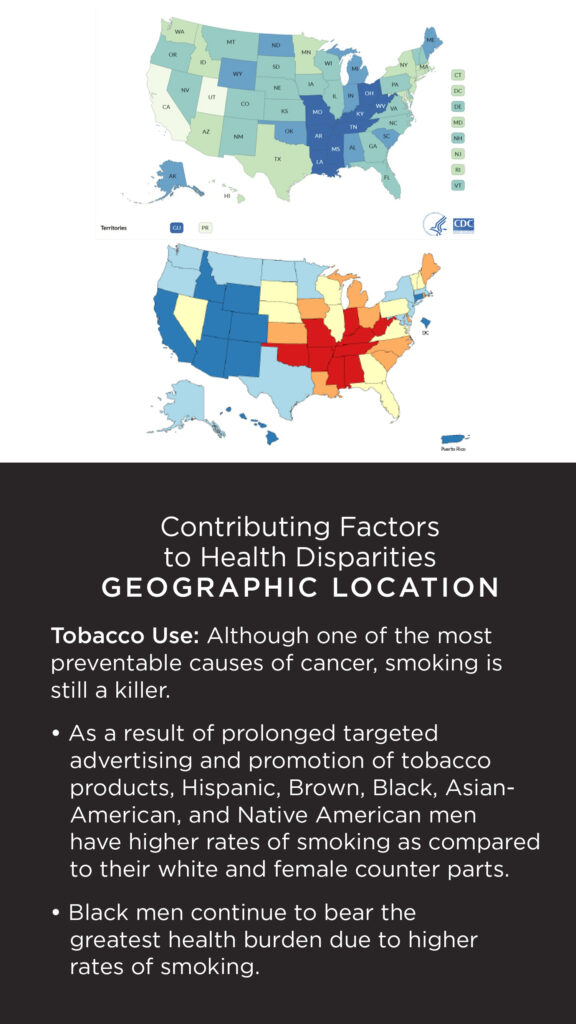
Slide #11
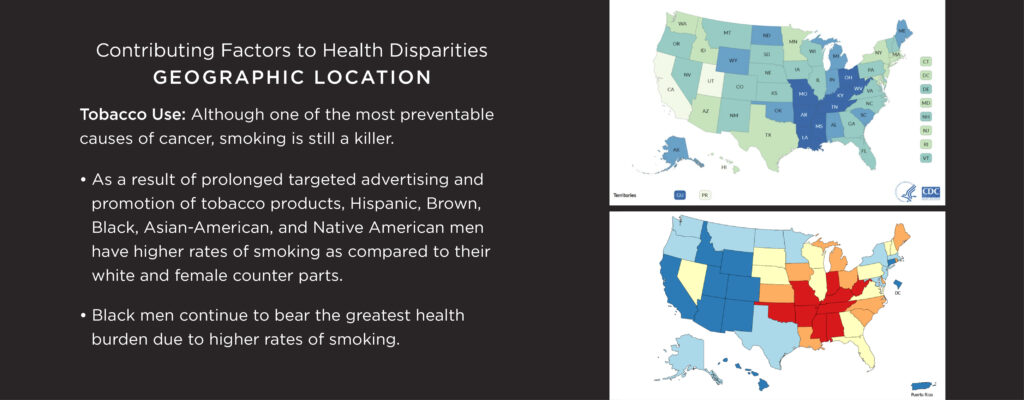
Top map Citation: https://www.cdc.gov/statesystem/cigaretteuseadult.html
Bottom map Citation: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6254a3.htm?s_cid=mm6254a3_w
Native Americans Citation: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6254a3.htm?s_cid=mm6254a3_w
To Learn More
There are many studies and reports about other populations and factors that influence cancer rates, including education, age, sexual orientation, gender identity, disability, housing status, national origin, and/or other characteristics. Below are links to some of these important studies:
NIH Report: What Are Health Disparities and Health Equity? We Need to Be Clear
CDC Report: Cancer Screening Prevalence Among Adults with Disabilities
CDC Report: Cancer Within American Indian and Alaska Native (AI/AN) Populations
CDC Report: How Racism Leads to Cancer Health Disparities
For more information about disparities of care leading to health inequity, the following conversations from the 2021 and 2022 National Cancer Prevention Workshops, hosted by Less Cancer, provide valuable insight and information on a range of issues.
2021 John Dingell Disparities and Inequities in Cancer Panel
2022 John Dingell Disparities and Inequities in Cancer Panel
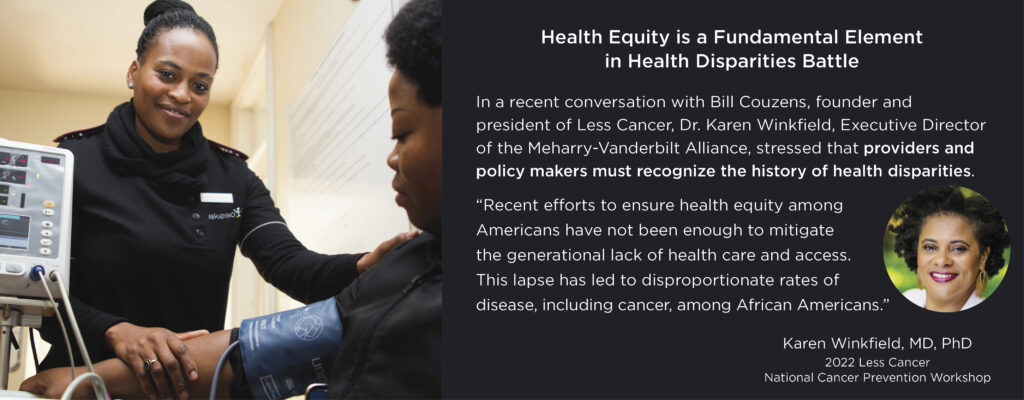
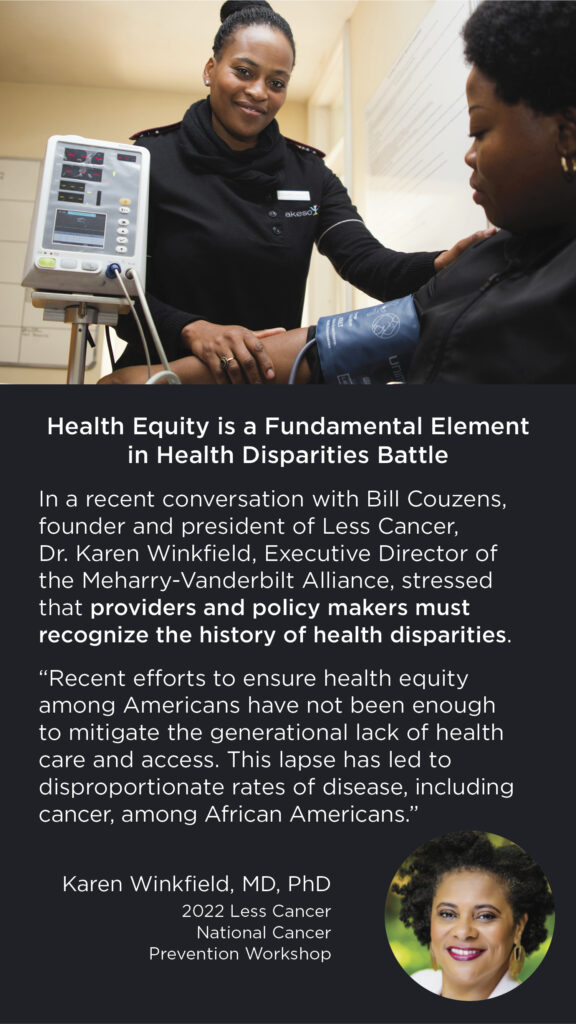
Dr. Karen Winkfield, Executive Director, Meharry-Vanderbilt Alliance
Dr. Mona Hanna-Attisha, Founder and Director, Michigan State University and Hurley Children’s Hospital Pediatric Public Health Initiative; Author, What the Eyes Don’t See
Tabitha Brown, Actress and Vegan Lifestyle Leader, discusses Food and Healthy Choices in the Prevention of Cancer
Robert Bilott, JD, Board Member, Less Cancer Board of Directors; Partner, Taft, Stettinius & Hollister LLP; Author, Exposure: Poisoned Water, Corporate Greed, and One Lawyer’s Twenty-Year Battle against DuPont (feature film, Dark Waters) on the impact of contaminants on rural, low-income communities