
Photo by Cody Pope/Vector Center
What increases your risk of getting cancer? Is perception aligned with reality?
This is Part Two of three articles revealing results of a study by Vector Center for Less Cancer’s National Cancer Prevention Day Workshop.
Alcohol
Is reality data aligned with public perception about links between cancer and alcohol?
The International Agency for Research on Cancer (IARC) division of the World Health Organization classifies chemical substances into 5 categories, based upon the likelihood that they cause cancer in humans. The worst of the worst — known carcinogens — are “Group 1.” Group 1 includes toxins like asbestos, plutonium, and coal-tar. It is no surprise to see arsenic, benzene and formaldehyde on this list. DDT did not make Group 1 — it is not carcinogenic enough. Yet, it may surprise you to learn that alcoholic beverages are Group 1 known carcinogens.
Evidence-based science tells us that consuming alcoholic beverages increases your risk of cancer. This science was first recognized in the 20th Century, and thousands of scientific studies since have revealed the strong link between alcohol consumption and certain cancers.
As reported by the National Cancer Institute, alcohol consumption, even moderate, increases risk of cancers including at least breast, head & neck, esophageal, liver, and colorectal. According to the American Society of Clinical Oncology (ASCO), consuming one 8oz alcoholic beverage per day for women (or two for men), doubles your risk of mouth and throat cancers and more than doubles risk of esophageal cancer. The cancer risk is related to the alcohol itself (these beverages contain ethanol which is a Group 1 substance). It is also related to how your body processes alcoholic beverages by breaking down ethanol into toxic acetaldehyde (another Group 1 substance).
Mapping alcohol consumption rates in America reported from 2012–2002, we see that Utah has the lowest drinking rate at nearly 27% of the adult population and the drinking rate rises to 68% of adults in the states with the highest rate. There are 22 states with higher percentages of adults who drink.

Adult Drinking Habits 2012, source Institute for Health Metrics and Evaluation (IHME). http://www.healthdata.org/alcohol
So, what do people believe? Do people understand the link between drinking and cancer? People now know smoking tobacco and sun exposure cause cancer, due to strong public education campaigns.
Using Vector Center analytics, powered by artificial intelligence (AI), we have compared state alcohol consumption rates to people’s perception of alcohol and cancer. Vector Center analyzed millions upon millions of media articles and social media postings from January 2016 to the present to determine whether people associate alcohol and cancer. Despite that 22 states pop in darker blues on the map of adult alcohol consumption as having higher drinking rates, Vector Center analytics reveal that only 4 states show higher perception that alcohol is a risk factor for cancer, as measured by volume of articles and posts. Most states have low perception of this cancer risk:
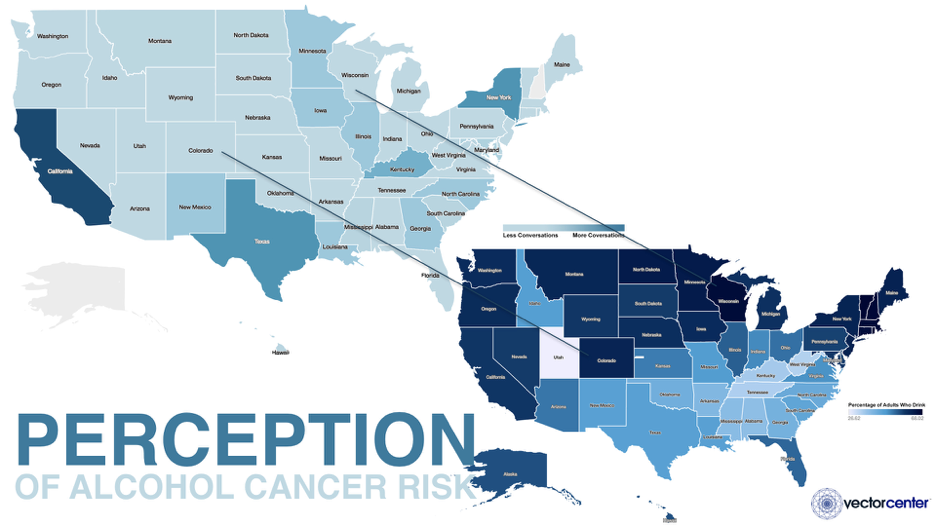
Colorado and Wisconsin show low volume of media articles and social media postings linking alcohol and cancer, yet have some of the highest drinking rates of 63% in Colorado and nearly 68% in Wisconsin. Only 30% of Americans cited alcohol consumption as a cancer risk factor in the ASCO National Cancer Opinion Survey dated October 24, 2017.
Despite evidence-based science showing that there exists a strong link between drinking alcoholic beverages and certain cancers, and this is a modifiable behavior, ASCO self-admittedly did not address this topic until January 1, 2018. On January 8, 2018, The Guardian reported that in the U.K. only 1 in 10 people know alcohol can cause cancer, despite that Europe, including the U.K., has by far the highest drinking rates in the world, as reported by the World Health Organization in its 2014 Global Status Report on Alcohol and Health and the IARC Monographs on the Evaluation of Carcinogenic Risks to Humans in 2010.
Perception is not aligned with reality. Why not?
Consider the Mad Men era when people smoked at work, in their cars, even in bed. Society did not want to believe that smoking caused cancer. Society did not want to change behavior. If it weren’t for evidence-based science leading the way into a strong public education campaign, perception about the link between smoking and cancer would not have changed.
Perhaps the same is true with alcohol consumption. People do not want to equate this vice, this social activity, with cancer.
The gap between perception and reality reveals a disconnect between science and public knowledge, and an opportunity to bridge this gap with a strong public education campaign.
The future in cancer prevention will include harnessing the Fourth Industrial Revolution (4IR) power of big data analytics for statistical analysis of cancer rates and their correlation to risk factors. AI may be used to track in real-time public awareness of risk factors for modifiable behaviors, such as alcohol consumption, to allow for course correction. Certainly, the future in cancer prevention critically relies on effective communication of evidence-based science.
Vector Center provides decision-grade intelligence in real-time to manage business disruptions. Our unique Perception Reality EngineTM technology uses AI to analyze millions of reality, perception and context data points in real-time to provide insights and strategies for business growth at the intersection of water, food and energy.

Leave A Comment
You must be logged in to post a comment.